Medical technology has come a long way. From stethoscopes to MRIs, each step has changed how we understand and treat patients. And now, it’s moving into a whole new dimension. Augmented Reality, or AR, isn’t like Virtual Reality. VR takes you somewhere else. AR keeps you here but adds a digital layer on top. In healthcare, that means surgeons can see organs and blood vessels in 3D on the patient’s body, or patients can understand their conditions better by seeing them come to life.
This isn’t just futuristic hype. WHO’s global strategy already highlights AR as a tool that can strengthen healthcare systems. FDA approvals show it’s safe and practical, moving into real hospitals today. Across education, diagnostics, surgery, and rehab, AR is quietly reshaping healthcare, and this article dives into how it’s happening every step of the way.
Enhancing Patient Understanding and Engagement with AR
Let’s be honest, traditional patient education can be confusing. Complex diagrams, medical jargon, and endless explanations leave most patients guessing. AR in healthcare flips that script. Point an AR device at a patient and suddenly, their organs, their condition, their treatment plan appear in 3D. They don’t just hear about it, they see it, understand it, and connect with it.
It’s not just a visual gimmick. AR apps let patients explore chronic conditions interactively. Someone managing diabetes can see exactly how exercise, diet, or medication affects their glucose levels. Rehab exercises, treatment steps, even surgical procedures become tangible experiences instead of abstract instructions. Patients interact, experiment, and learn in real time.
NHS pilot programs confirm this impact. They show that AR visualizations significantly improve patient understanding and treatment compliance. Patients leave consultations with clarity and confidence. They follow treatment plans more reliably and feel less anxious about their care.
The real magic of AR is how it transforms learning into a journey. Education is no longer passive; it’s active, engaging, and human-centered. Patients become partners in their own healthcare, bridging the gap between complex medical knowledge and real understanding. AR is not a futuristic idea, it’s a tool that is already reshaping the patient experience.
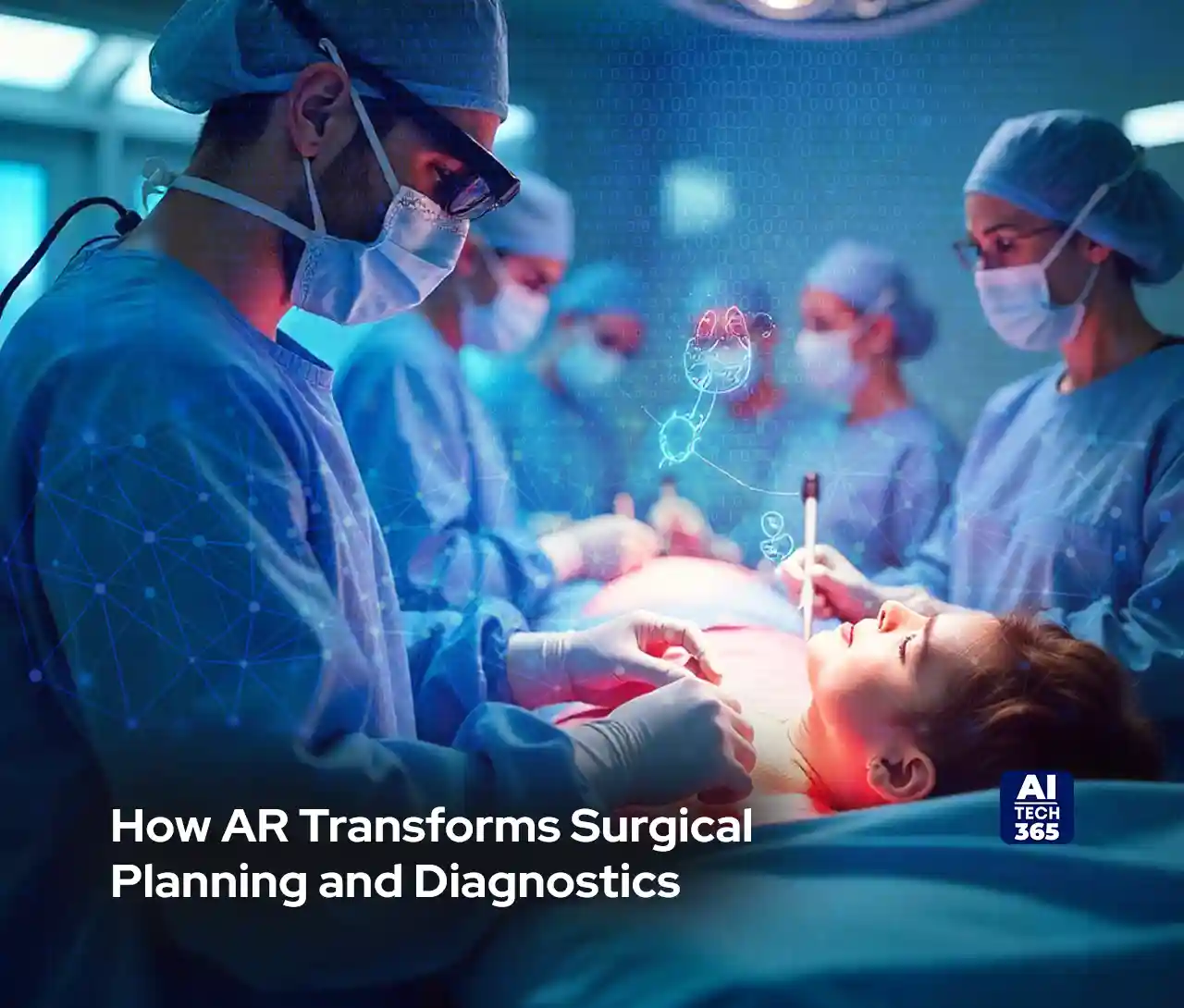
How AR Transforms Surgical Planning and Diagnostics
Surgery is unforgiving. One small misstep, and things go sideways fast. That’s where AR in healthcare steps in. Surgeons can literally see inside the patient before cutting with the help of CT scans, MRI results, all overlaid in 3D on the body. Tumours, nerves, blood vessels, they’re right there. You don’t just plan; you experience the operation first.
Planning with AR is not about saving time, it’s about clarity. The surgeons can study the tricky anatomy virtually and anticipate snags so as to carry out every step before coming into the operating room (OR). The FDA has approved certain AR diagnostic overlays that allow clinicians to visualize complex anatomy in time, reducing errors and making planning more efficient. That’s not a small win, that’s life-saving precision.
And it doesn’t stop there. Minimally invasive and robot-assisted surgeries get a huge boost. Virtual guides show exactly where instruments should go. Surgeons still use their hands, but now they have a digital roadmap. Operations are cleaner, recovery is faster, and mistakes happen less often.
This isn’t a theory or a distant future. FDA-approved AR devices are already proving themselves in hospitals. Spinal surgeries, complex abdominal procedures, they’re seeing measurable improvements, fewer errors, and more predictable results.
At the end of the day, AR turns guesswork into confidence. Surgeons get clarity. Patients get better outcomes. Hospitals run smoother. If you’re still relying on old-school planning, you’re leaving precision and safety on the table. AR isn’t coming. It’s here.
Precision in the Operating Room with AR
Once the surgery starts, every second counts. AR in healthcare gives surgeons a heads-up display they never had before. Virtual guides projected onto the patient show exactly where tumors, nerves, and blood vessels are. You’re not guessing, you’re navigating with precision.
Minimally invasive and robot-assisted procedures benefit hugely. Instruments glide where they should, surgical paths are clear, and critical structures are avoided. Surgeons still rely on their skill, but AR acts like a second pair of eyes; always accurate, always on. NHS reports show AR-assisted surgeries increase procedural accuracy and reduce complications in minimally invasive and complex surgeries. That’s not a small improvement. That’s patient safety, redefined.
Early trials highlight the difference. Spinal surgeries guided by AR have fewer misplacements. Complex abdominal procedures are more predictable. Recovery is smoother, and the risk of post-op complications drops. AR isn’t just an accessory; it’s part of the surgical toolkit now.
Beyond accuracy, AR saves mental bandwidth. Surgeons can focus on decision-making instead of constantly interpreting 2D scans. Real-time overlays make the operating field intuitive. They see what’s under the surface without making extra cuts, and they make confident choices on the fly.
Hospitals that implement AR report not only improved outcomes but also increased team coordination. Nurses, anesthesiologists, and assistants can look at the same overlays, anticipate the next step, and act in union. The technology assures that the OR ceases being a high-pressure guessing game into a guided, precise operation.
At the end of the day, AR in healthcare turns complexity into control. Surgeons get clarity, patients get safety, and hospitals get efficiency. This is the surgical superpower that was once science fiction. Now, it’s real and it’s saving lives.
Also Read: Genie 3 by DeepMind: Real-Time 3D Worlds from a Single Text Prompt
Rehabilitation and Training with AR
AR in healthcare doesn’t stop when the surgery ends. It steps into rehab and training, turning what used to be boring, repetitive exercises into interactive experiences. Imagine a stroke patient doing physical therapy while seeing progress, targets, and real-time feedback projected in front of them. Movements become a game, motivation spikes, and exercises actually get done.
Cognitive rehabilitation benefits too. Patients recovering from traumatic brain injuries can interact with visual overlays that guide memory exercises, problem-solving tasks, and coordination drills. The therapy is no longer abstract, it’s tangible, engaging, and personalized.
Medical training also gets a massive upgrade. Students can practice complex procedures on holographic models, seeing anatomy in 3D without risking a real patient. Repetition, trial and error, and mistakes become safe learning tools.
WHO and NHS evidence show AR gamification boosts patient motivation and adherence in rehab programs while improving training outcomes for medical students. It’s not just a tech novelty; it’s a human-centered tool that improves results, keeps patients committed, and prepares future surgeons with confidence.
AR in this space proves the technology touches every stage of healthcare, from recovery to skill-building, making both patients and professionals more engaged and capable.
Overcoming Challenges and Looking Ahead
AR in healthcare is amazing, but it’s not all easy. Costs are high, rules are strict, data privacy is tricky, and staff need proper training. Hospitals can’t just roll it out overnight. WHO points out that things like regulatory compliance, infrastructure gaps, and the need for skilled users’ slow adoption down.
Even so, the potential is huge. FDA guidance says that once scaled, AR devices could be as common as an MRI or X-ray. At the heart of the new experiences would be malignancies working the leaflet.
Paradoxically, prices have dropped, and training has improved; the regulators are not sitting idly by-their regulations are coming into shape, now. The AR is going from something cutting-edge into a commonplace. Now, better, smarter, safer patient care is delivered; the healthcare team. It gives them actual tools to do their jobs.
The Future is Here
AR isn’t just a flashy idea anymore. It’s helping patients actually understand their conditions, making diagnostics clearer, and giving surgeons real precision during operations. And it doesn’t stop there, rehab, training, and day-to-day healthcare are all seeing its impact.
It’s not theory or hype. WHO strategies back it, and FDA approvals show it works in real hospitals today. AR is already changing how medicine is taught and delivered. The tools are here, the results are real, and the future of healthcare is looking augmented; smarter, safer, and more precise every day.